Raw Milk Institute (RAWMI) recently traveled to Pennsylvania and Delaware in support of low-risk raw milk. Through training farmers, meeting with regulators, and visiting farms, we’re aiming to help ensure that raw milk is safe, embraced, and accessible in the northeastern states.
BUILDING BRIDGES WITH REGULATORS AND FARMERS IN DELAWARE
RAWMI President Mark McAfee and Vice President Sarah Smith met with Delaware Secretary of Agriculture Don Clifton, alongside dairy farmers Steph and Gregg Knudsen, to discuss Delaware's recent raw milk legalization, proposed regulations, and ways we can all collaborate to ensure accessibility to safe raw milk in Delaware.
The Knudsens were instrumental in getting the legalization Bill passed so that more farms can thrive in Delaware. Mark and Sarah visited their G&S Dairy Farm to talk about the path moving forward now that raw milk is legal.
EDUCATING FARMERS FOR A SUSTAINABLE PATH FORWARD
Mark McAfee, Sarah Smith, and Dr Joseph Heckman taught a 3-hour seminar on World Class Raw Milk at the PASA Sustainable Agriculture Conference in Lancaster, Pennsylvania. Topics included
History of raw milk
Why raw milk farms are thriving
Health benefits of raw milk
Benefits of selling raw milk
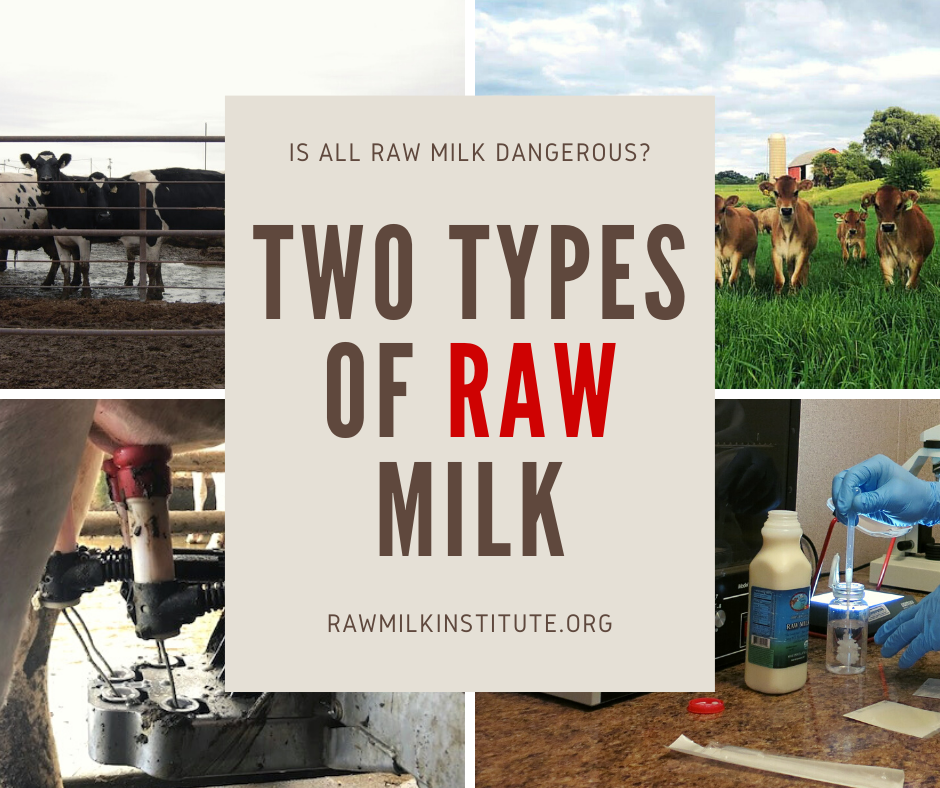
Safety and risks of raw milk
Grass-to-glass raw milk risk management
Raw milk testing
There were ~45 attendees from Pennsylvania, New Jersey, New York, Maryland, and Delaware. Attendees included farmers who are already producing raw milk, prospective farmers considering raw milk production, and students who were interested to know more about raw milk.
THANKS to Lancaster Farming newspaper for giving balanced coverage of this raw milk training class and the potential benefits of raw milk production for farmers. https://www.lancasterfarming.com/farming-news/dairy/demand-for-raw-milk-offers-opportunities-for-farmers/article_7b69a814-e401-11ef-93cf-b332916b01d8.html
PIONEERING FOR LOW-RISK RAW MILK
Edwin Shank, from The Family Cow dairy in Chambersburg Pennsylvania, is the farmer who pioneered on-farm bacterial testing for raw milk dairies. We're always happy to visit with Edwin and see how his multigenerational family farm is thriving. Edwin's farm is RAWMI Listed and we share his on-farm lab educational materials here: https://www.rawmilkinstitute.org/updates/on-farm-lab-testing-for-raw-milk-farmers
CONNECTING WITH AMISH FARMERS
There are many dozens of Amish dairies, but they can't generally access RAWMI’s online training materials. We want to make sure they have access to the information they need for low-risk raw milk production, regardless of any barriers to technology.
Several Amish farmers attended our training class in Lancaster, and we visited several Amish farms that are thriving with the current cultural shifts towards food security, local producers, and healthier foods to nourish the gut microbiome and immune system.
Overall, this trip was a resounding success! We were gratified to train more farmers in low-risk raw milk production and look forward to future collaboration towards successful rollout of Delaware’s recent raw milk legalization.