Government-Funded Study Finds ZERO Pathogens in Raw Milk Samples!
That’s what the headlines should have read.
Instead, the study was titled, “Reservoirs of antimicrobial resistance genes in retail raw milk” [1]. The study, funded by the National Institutes of Health (NIH) and the United States Department of Agriculture (USDA), was not able to find any pathogens in raw milk. So instead they focused on trying to create fear of antibiotic resistant genes which were found to proliferate when raw milk was allowed to sit at room temperature for hours.
Antibiotic Resistant Genes are Ubiquitous
Antibiotic resistant genes are everywhere. They’ve been found in every environment, including pristine habitats that have been virtually untouched by humans such as Antarctica [2, 3]. They’re even found in the dust of buildings [4].
“Antibiotics are ancient, dating back hundreds of millions of years. Resistance is therefore equally ancient, and the number of genes in the resistome is a reflection of the continuous co-evolution of small molecules in natural environments and microbial genomes.”
-Gerard Wright, Nature Reviews Microbiology 2007 [3]
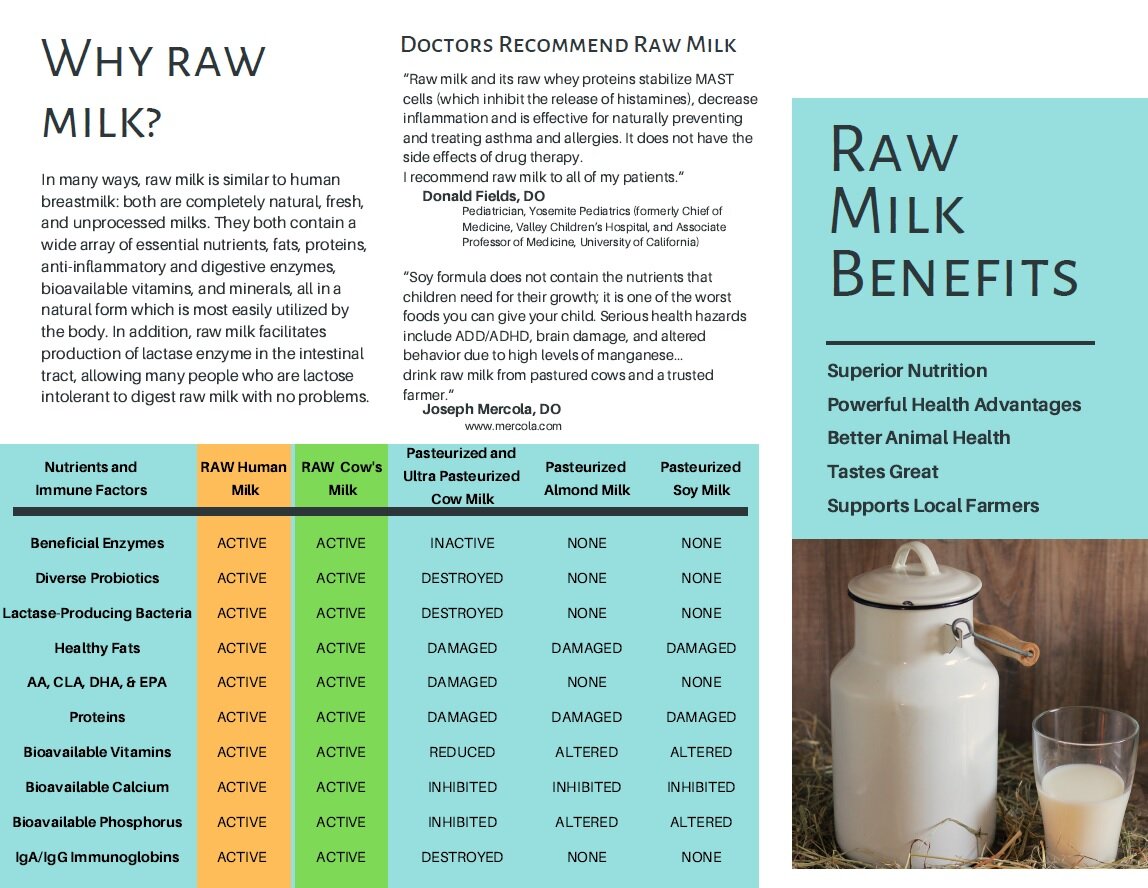
Given that they are ubiquitous in the environment, it is no surprise that there are antibiotic resistant genes in many foods [5]. Breast milk, too, contains antibiotic resistant genes carried on bacteria found in the raw breast milk [6].
Breastmilk and Antibiotic Resistant Genes
Researchers in Helsinki found that, even though breast milk contains antibiotic resistant genes, babies who were breast fed actually have less antibiotic resistant genes in their guts than babies who weren’t breastfed or who terminated breastfeeding early [7]. Researchers attribute this benefit to the fact that breastmilk promotes the growth of beneficial bacteria such as bifidobacteria, which can then outcompete the bacteria carrying antibiotic resistant genes. Like breast milk, cow’s milk has also been shown to support the growth of bifidobacterial [8].
Potential Dangers of Antibiotic Resistant Genes
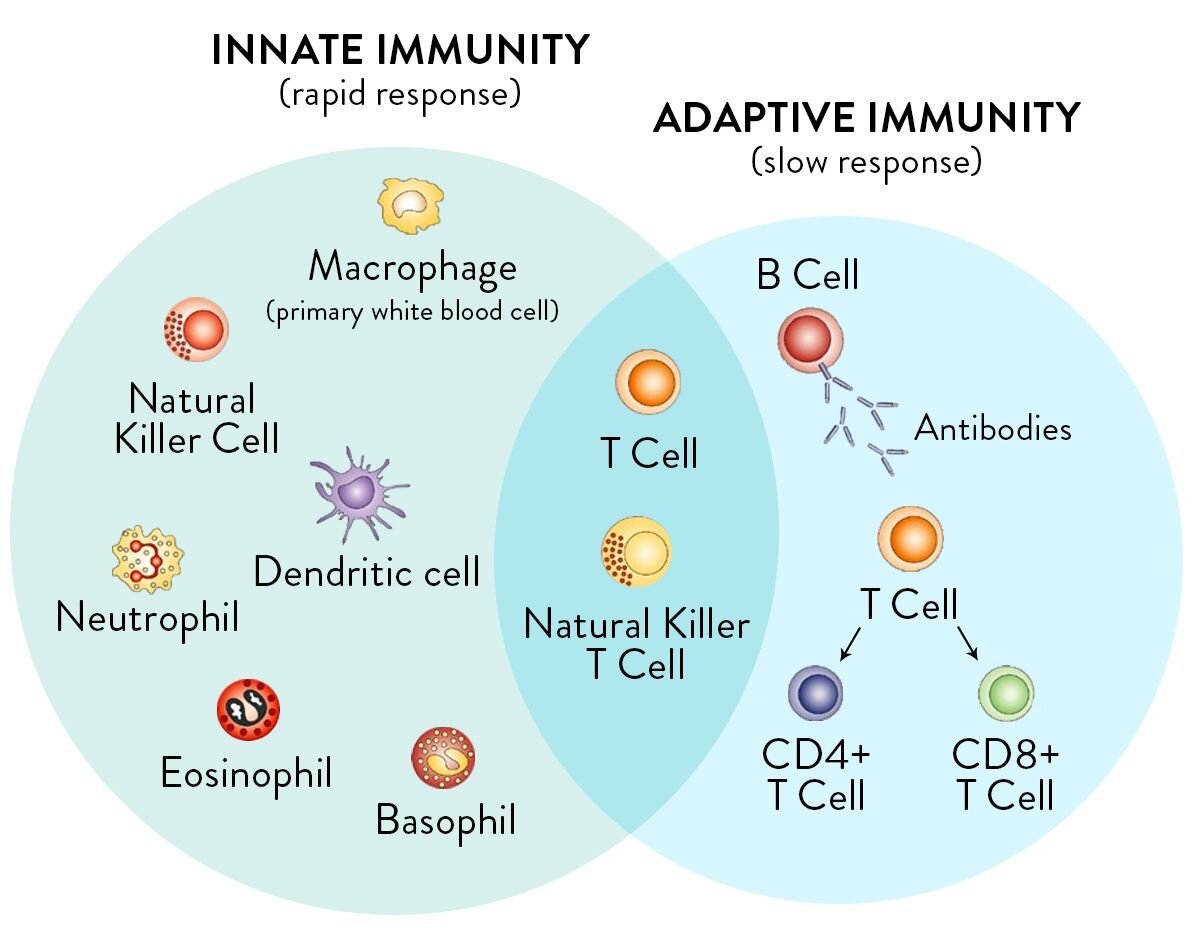
Antibiotic resistant genes can pose potential health threats in specific circumstances. When antibiotics are taken, the intestinal microbiome is disrupted as both beneficial and harmful bacteria are killed off. This weakens our immune systems overall [9]. If there are antibiotic resistant bacteria present in the gut, taking antibiotics actually allows these bacteria to proliferate in the absence of competing bacteria. There can then be infection or illness which is not able to be respond to antibiotics. Antibiotic resistance is now responsible for the deaths of tens of thousands of people every year in the USA alone [10].
For example, C. diff. colitis (clostridium difficile colitis) is infection of the colon that results from disruption of the healthy bacteria in the gut, usually as a result of taking antibiotics. C. diff. can cause diarrhea, abdominal pain, fever, bloody stools, kidney failure, and even death. One of the best treatment options for severe C. diff. infections is fecal transplant. Severely ill C. diff. patients have a 92% cure rate from fecal transplants, which provide a healthy flush of poop from a healthy human donor into the colon [11]. The fecal transplant recolonizes the gut with healthy bacteria.
Zero Pathogens in Raw Milk Samples
Coming back to the study funded by the NIH and USDA [1], researchers found that antibiotic resistant genes proliferated in raw milk that was allowed to sit at room temperature for hours. Their research showed that raw milk which was kept refrigerated had low levels of antibiotic resistant genes. What this actually demonstrates is that raw milk from around the country is being produced very cleanly, resulting in low bacteria counts.
Most of the potential beneficial bacteria to be found in milk is from either fecal or soil origin. Yes…dirt is very good for you and a little poop does not hurt either [12]. It has long been understood that living in a farm environment has substantial health benefits over living in urban environments [13]. However, in our modern world with immune-compromised consumers, the raw milk standards have had to change.
For raw milk to be legal for sale and safe for the general public (including immune-compromised people), it must be very hygienic. It can no longer have dirt or poop in it. So, all that is left is clean, delicious, safe raw milk from deep inside the cow’s or goat’s udder. The government-funded study tested retail raw milk samples and they found ZERO pathogens! This should be celebrated as true progress towards farm cleanliness and testing.
“[Raw] milk samples in the present study were screened for Listeria spp., Salmonella enterica, and E. coli O157:H7. None were detected.”
-Liu et al. Microbiome 2020 [1]
Fermenting Raw Milk
For thousands of years, people have known how to ferment or “clabber” raw milk by simply leaving it at room temperature instead of refrigerating it. In the absence of refrigeration, traditional cultures often consumed raw milk in fermented form [14]. Such milk would have contained ample beneficial lactic acid bacteria from the small amounts of dirt or manure that would have been present on the udders and teats of the milk animals, and would therefore quickly ferment at room temperature.
In modern times, people have largely lost their taste for spontaneously fermented, sour raw milk. Raw milk farmers and consumers aim to maintain the sweet flavor of fresh milk as long as possible. The farmers do this by thoroughly cleaning the udders and milking equipment to ensure the milk will have low bacteria counts [15], as well as by rapidly chilling the milk and keeping it cold. Consumers, too, work to make sure their raw milk is kept cold, even during transport. Keeping raw milk cold allows it to retain its sweet taste and gives it a longer shelf life.
One useful point of information from the government-funded study was the finding that “spontaneous fermentation does not grow beneficial lactic acid bacteria”. This means that the very clean, low-bacteria count raw milk which is currently available in the USA may not ferment very well in the traditional way. The flavor of spontaneously fermented raw milk is not generally palatable to the modern raw milk consumer. Thus, most raw milk consumers actually work to make sure that their raw milk does not ferment and stays fresh and sweet.
Generally, raw milk consumers who intentionally ferment their milk will do so by adding beneficial bacteria such as yogurt starter or kefir grains. Kefir, in particular, is associated with a wide number of health benefits including lower blood pressure, decreased insulin resistance, tumor suppression and prevention, and improved composition of the gut microbiota [16-19].
The Bottom Line
The NIH and USDA-funded study found no pathogens in raw milk. This is further confirmation of the findings published in the January 2020 Journal of Epidemiology and Infection which concluded that “raw milk can be produced with a high level of hygiene and safety” [20].
The government-funded study focused on antibiotic resistant genes which can proliferate in raw milk that is left at room temperature for hours. However, it is no surprise that raw milk, like breastmilk and many other foods, contains antibiotic resistant genes. The presence of antibiotic resistant genes is not an issue unless the balance of good bacteria in the gut gets disrupted. Both breastmilk and raw milk are known to promote the growth of beneficial bacteria such as bifidobacteria. The study completely ignored the growing body of evidence that has shown that children who drink raw milk have decreased rates of asthma, allergies, eczema, ear infections, fever, and respiratory infections [21-23].
The best way to beat antibiotic resistant bacteria is to protect and nourish the biodiverse bacteria in the gut. You can do this by avoiding antibiotics and processed foods, which damage the gut and immune system [24, 25]. Instead, eat plenty of whole foods such as raw milk, milk kefir, grassfed beef, eggs, and fresh or fermented vegetables and fruits to feed the beneficial bacteria in the gut and allow it to thrive [26].
References
[1] Liu, J., Zhu, Y., Jay-Russell, M. et al. (2020) Reservoirs of antimicrobial resistance genes in retail raw milk. Microbiome 8, 99 (2020). https://doi.org/10.1186/s40168-020-00861-6
[2] Durso LM, Miller DN, Wienhold BJ (2012) Distribution and Quantification of Antibiotic Resistant Genes and Bacteria across Agricultural and Non-Agricultural Metagenomes. PLOS ONE 7(11): e48325. https://doi.org/10.1371/journal.pone.0048325
[3] Wright, G. (2007) The antibiotic resistome: the nexus of chemical and genetic diversity. Nat Rev Microbiol 5, 175–186 (2007). https://doi.org/10.1038/nrmicro1614
[4] Ben Maamar S, Glawe AJ, Brown TK, Hellgeth N, Hu J, et al. (2020) Mobilizable antibiotic resistance genes are present in dust microbial communities. PLOS Pathogens 16(1): e1008211. https://doi.org/10.1371/journal.ppat.1008211
[5] Fogler K, Guron GKP, Wind LL, Keenum IM, Hession WC, Krometis L-A, Strawn LK, Pruden A and Ponder MA (2019) Microbiota and Antibiotic Resistome of Lettuce Leaves and Radishes Grown in Soils Receiving Manure-Based Amendments Derived From Antibiotic-Treated Cows. Front. Sustain. Food Syst. 3:22. doi: 10.3389/fsufs.2019.00022
[6] Pärnänen, K., Karkman, A., Hultman, J. et al. (2018) Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat Commun 9, 3891. https://doi.org/10.1038/s41467-018-06393-w
[ 7] Ravindran S. (2019) Breastfeeding May Help Protect Babies from Antibiotic-Resistant Bacteria. SPLASH! milk science update: January 2019 Issue. https://milkgenomics.org/article/breastfeeding-may-help-protect-babies-from-antibiotic-resistant-bacteria/
[8] Rova S, Rada V, Marsik P, Vlkova E, Bunesova V, Sklenar J, Splichal I. (2011) Growth of bifidobacteria and clostridia on human and cow milk saccharides. Anaerobe 17(5). https://doi.org/10.1016/j.anaerobe.2011.07.009.
[9] McAfee M, Smith S. (2020) Immunity, the Immune System, and Raw Milk. Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/immunity-the-immune-system-and-raw-milk
[10] Centers for Disease Control and Prevention. (2019) More People in the United States Dying from Antibiotic-Resistant Infections than Previously Estimated. CDC website. https://www.cdc.gov/media/releases/2019/p1113-antibiotic-resistant.html
[11] Brandt L. J. (2012). Fecal transplantation for the treatment of Clostridium difficile infection. Gastroenterology & hepatology, 8(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3365524/
[12] Akst, J. (2020) The influence of soil no immune health. The Scientist website. https://www.the-scientist.com/news-opinion/the-influence-of-soil-on-human-health-66885
[13] Wells, AD, Poole JA, and Romberger DJ. (2014) Influence of farming exposure on the development of asthma and asthma-like symptoms. International immunopharmacology, 23(1), 356–363. https://doi.org/10.1016/j.intimp.2014.07.014
[14] Levi, J. (2014) The Smoke Cured Fermented Milk of the Samburu. Presentation at Wise Traditions London 2014. https://westonaprice.london/videos/samburu/
[15] Smith, S. (2020) Udder Preparation for Raw Milk. Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/udder-preparation-for-raw-milk
[16] Bourrie BC, Willing BP, and Cotter PD. (2016) The Microbiota and Health Promoting Characteristics of the Fermented Beverage Kefir. Frontiers in microbiology, 7, 647. https://doi.org/10.3389/fmicb.2016.00647
[17] Bellikci-Koyu E, Sarer-Yurekli BP, Akyon Y, Aydin-Kose F, Karagozlu C, Ozgen AG, Brinkmann A, Nitsche A, Ergunay K, Yilmaz E, and Buyuktuncer Z. (2019) Effects of Regular Kefir Consumption on Gut Microbiota in Patients with Metabolic Syndrome: A Parallel-Group, Randomized, Controlled Study. Nutrients, 11(9), 2089. https://doi.org/10.3390/nu11092089
[18] Guzel-Seydim ZB, Kok-Tas T, Greene AK, Seydim AC. (2011) Review: functional properties of kefir. Crit Rev Food Sci Nutr. 51(3):261-268. doi:10.1080/10408390903579029
[19] de Oliveira Leite AM, Miguel MA, Peixoto RS, Rosado AS, Silva JT, and Paschoalin VM. (2013) Microbiological, technological and therapeutic properties of kefir: a natural probiotic beverage. Brazilian journal of microbiology : [publication of the Brazilian Society for Microbiology], 44(2), 341–349. https://doi.org/10.1590/S1517-83822013000200001
[20] Berge AC, Baars T. (2020) Raw milk producers with high levels of hygiene and safety. Epidemiology and Infection. 148:e14. doi:10.1017/S0950268820000060
[21] Loss G, Apprich S, Waser M, Kneifel W, Genuneit J, Büchele G, Weber J, Sozanska B, Danielewicz H, Horak E, Joost van Neerven RJ, Heederik D, Lorenzen PC, von Mutius E, Braun-Fahrländer C; GABRIELA study group. (2011) The protective effect of farm milk consumption on childhood asthma and atopy: The GABRIELA study. Journal of Allergy and Clinical Immunology. 128 (4): 766-73. https://www.jacionline.org/article/S0091-6749(11)01234-6/fulltext
[22] Perkin MR and Strachan DP. (2006) Which aspects of the farming lifestyle explain the inverse association with childhood allergy? Journal of Allergy and Clinical Immunology. 2006; 117 (6):1374-81. https://www.jacionline.org/article/S0091-6749(06)00651-8/fulltext
[23] Loss G, Depner M, Ulfman LH, Joost van Neerven RJ, Hose AJ, Genuneit J, Karvonen M, Hyvärinen A, Kaulek V, Roduit C, Weber J, Lauener R, Pfefferle PI, Pekkanen J, Vaarala O, Dalphin JC, Riedler J, Braun-Fahrländer C, von Mutius E, Ege MJ; PASTURE study group. (2015) Consumption of unprocessed cow's milk protects infants from common respiratory infections. Journal of Allergy and Clinical Immunology. 135 (1): 56-62. https://www.jacionline.org/article/S0091-6749%2814%2901274-3/fulltext
[24] Watanabe K, Gilchrist CA, Uddin J, Burgess SL, Abhyankar MM, Moonah SN, Noor Z, Donowitz JR, Schneider BN, Arju T, Ahmed E, Kabir M, Alam M, Haque R, Pramoonjago P, Mehrad B, Petri WA. (2017) Microbiome-mediated neutrophil recruitment via CXCR2 and protection from amebic colitis. PLOS Pathogens; 13 (8): e1006513 DOI: 10.1371/journal.ppat.1006513
[25] Paula Neto HA, Ausina P, Gomez LS, Leandro JGB, Zancan P, Sola-Penna M. (2017) Effects of Food Additives on Immune Cells As Contributors to Body Weight Gain and Immune-Mediated Metabolic Dysregulation. Front Immunol.8:1478. doi:10.3389/fimmu.2017.01478
[26] McAfee M. (2020) Build Immune System Strength With Whole Foods: Drink Raw Milk! Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/whole-foods-build-immune-system-strength