Why Did Ancient Humans Start Consuming Milk From Other Mammals?
10,000 years ago, early humans spent much of their time hunting, gathering, or fishing for food. Obtaining food was the dominant preoccupation of their lives. Imagine the reality for humans living prior to the advent of civilization. You can picture them living in crude shelters, wearing animal skins and using few tools. It was not like a 14-day survival challenge where they could call for a medic and be rescued. Eating and surviving were lifelong challenges.
You can hear the crying of babies and children that were hungry. Those cries are universal and have not changed over the millennia. The natural instinct to provide for the next generation was a compelling mandate which drove instinctual and natural innovation.
Early humans nursed their young, just as all mammals do. Nursing provided optimal nutrition for babies to survive and thrive. Breastmilk is a form of raw milk, serving as a complete food source that is perfectly designed to sustain life.
People observed animals in the wild nursing their young just as they nursed their own young. By capturing goats and aurochs (ancestral cow breeds), the people were able to collect their milk in pottery vessels. These humans would have learned quickly that milk from other animals was a complete, nutritious food. Being purposely designed to sustain life like no other food, this raw milk provided a steady source of readily available food for ancient humans.
Without refrigeration, any milk that wasn’t consumed quickly would naturally ferment into cheese curd and whey. The milk storage vessels likely contained bacteria cultures from previous milkings, and hence the culturing process was naturally reinforced with these bacteria. The resultant curds could be stored and consumed over time. Curd contained a complete set of microbiome-friendly nutrients, and would be easy to digest due to its biodiversity. The humans could now bring along with them a portable supply of steady food. As long as they had sunshine, water, grass or shrubbery, and a mammal, they had food.
Scientists have ample evidence that humans began drinking raw milk from animals at least 10,000 years ago. The evidence for the early use of animal milk is found in ancient clay pottery vessels, dental remains of Neolithic humans, and bone analysis of animal remains. Ancient baby bottles provide evidence that milk from animals was used to feed human infants at least 8,000 years ago.
The origin and dispersal of domestic livestock species in the Fertile Crescent. (Zeder, Melinda)
These agriculture-based civilizations were so successful that they spread across the Mediterranean region, Europe, Asia, and the Middle East over the next few thousand years. Humanity continued to domesticate additional species of animals; throughout history, many species have been utilized for their milk including camels, cows, goats, sheep, donkeys, horses, water buffalo, reindeer, and other mammals.
Those who consumed milk had a competitive advantage over those that did not have a steady source of readily available food. This steady supply of food allowed for settlements and communities to develop. People no longer had to spend most of their time acquiring food, and could instead use their brain power to drive the development of sophisticated structures and towns. Domesticated animals became high value assets. As civilization advanced, those that owned milking mammals became wealthy and became the source of food for communities.
Selection of late Bronze/early Iron Age feeding vessels.(J Dunne, et al.)
Lactase and Genetic Adaptations for Milk
The domestication of mammals and consumption of their raw milk provided a source of biodiverse colonies of bacteria for the human gut. When people began drinking raw milk at least 10,000 years ago, these biodiverse bacteria began the genomic adaptation for lactase production and lactase persistence genes. Lactase is the enzyme responsible for breaking down lactose into digestible form.
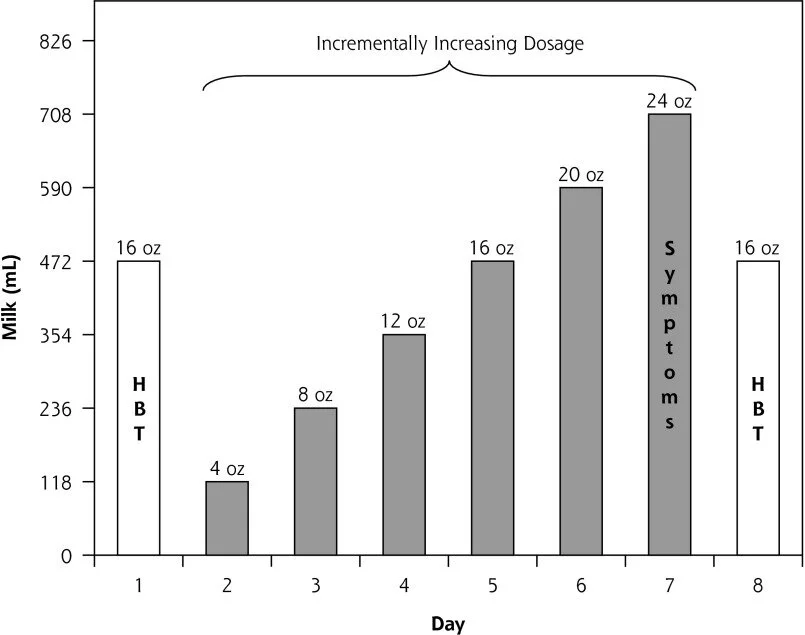
Humans who first began to consume milk from other mammals had not yet developed the lactase persistence gene. Nonetheless, they likely would have been able to readily digest raw milk because it facilitates the production of lactase enzyme in the intestinal tract. Archaeological evidence shows that humans were consuming raw milk for thousands of years before the widespread appearance of the lactase-persistence gene. This has led many researchers to the probably erroneous conclusion that Neolithic humans must have been fermenting or culturing milk to reduce or remove its lactose content.
In reality, “lactose-intolerance” is primarily pasteurization intolerance. Since raw milk facilitates the production of lactase, it is not likely that there were widespread issues with lactose intolerance in Neolithic populations. In all likelihood, these early populations would have been able to consume milk in its fresh form straight from the mammals, as well as in the lacto-fermented curds and whey which would form quickly without refrigeration.
Stone carving at the ancient Sumerian temple of Ninhursag showing typical dairy activities. (Dorling Kindersley, The Visual Dictionary of Ancient Civilizations)
The competitive advantage provided by raw milk is not to be understated. Raw milk allowed humans to thrive in conditions where survival would have been difficult. It allowed them to migrate and proliferate from region to region with a steady supply of food. Those populations that consumed milk further adapted by developing lactase-persistence genes. Scientists now believe that the lactase-persistence genes were spread through natural selection. This means that the reproductive capacity and/or survivability of ancient raw milk drinkers was substantially increased compared to non-milk-drinking populations. The lactase-persistence genes would have facilitated the easy digestion of milk in many forms, including boiled or cooked milk. There is current evidence of lactase persistence genes in people from regions of Africa, Europe, Asia, and the Middle East. However, even those without the lactase-persistent gene can generally digest raw milk because of the raw milk bacteria that create lactase for the human gut.
Pasteurization: A Technological Solution to a Manmade Problem
A 19th century illustration of "swill milk" being produced: a sickly cow being milked while held up by ropes. (Frank Leslie’s Illustrated Weekly)
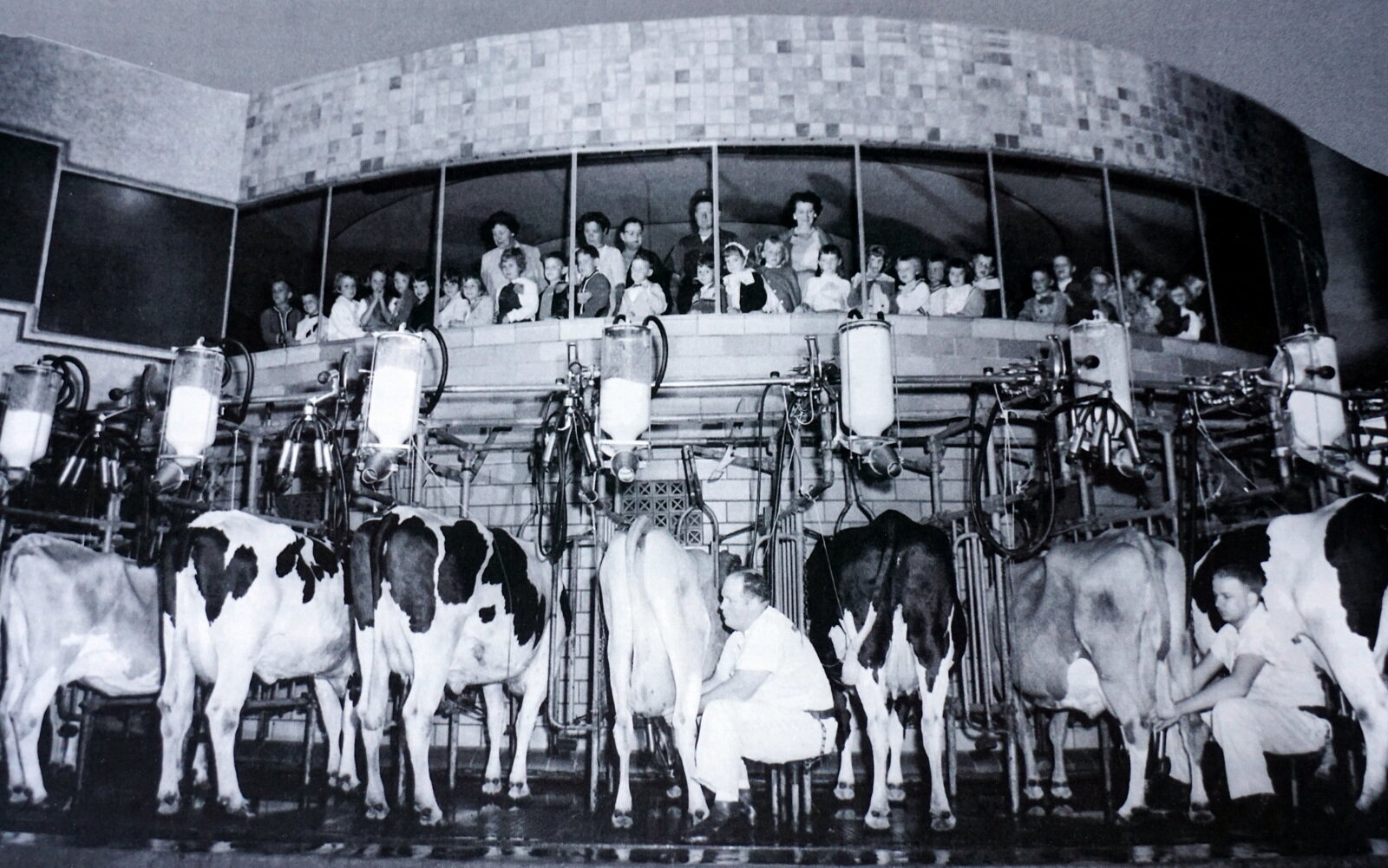
By the mid-1800’s in America, some raw milk production had shifted away from farms and into highly-populated cities. Big cities did not have pastures or clean water, and the cows in city dairies were kept in filthy conditions with poor nutrition and poor animal health. Many of these cows were fed byproducts from alcohol distilleries, leading to illness in the cows. Raw milk, which had been safely consumed by humans for nearly 10,000 years, had become a source of deadly diseases such as tuberculosis, typhoid, diphtheria, and scarlet fever.
In the late 1800's, it was recognized that raw milk being produced in these conditions was dangerous, and two solutions were proposed. Pasteurization was one of the solutions which was proposed to eliminate pathogenic bacteria in the milk coming from these filthy conditions. The other solution was to actually produce the milk in hygienic conditions with healthy animals.
It was known that raw milk was a superior source of nutrition for infants and children, so the American Association of Medical Milk Commissions (AAMMC) was established in the late 1800's to ensure a safe supply of hygienic raw milk. The AAMMC was in operation for nearly a century, certifying medical raw milk for use in hospitals and for feeding infants and children.
Pasteurization was ushered in to address filthy conditions and unhealthy cows in cities. It answered the question of how to commercialize dirty milk, rather than spending the time and energy it would take to produce clean milk from healthy cows. Clearly, over time, the pasteurization movement gained traction and became the standard for ensuring "safe" milk, yet pasteurization is known to degrade and damage many of the nutrients in milk.
Raw Milk’s Role in the 2020’s
Now in the 2020’s, we are in a time of widespread immune depression, comorbidities, and compromised health. For most Americans, the competitive advantage of raw milk consumption has never been a reality. Raw milk’s immune-building properties and microbiome friendly traits have been forgotten.
Instead, we live in the age of immune-destructive pharmaceuticals and antibiotics. Although life-saving in certain applications, these drugs also depress and damage the immune system and gut microbiome. Antibiotic resistance is now responsible for the deaths of tens of thousands of people every year in the USA alone. Furthermore, pasteurized milk is now recognized as a top food allergen and difficult to digest.
Raw milk is an innate part of our healthy immune history, and is largely missing in our sterile, sugar-laden, preservative-laced, antibiotic-abusing modern diets and medical culture. Safe raw milk has been rediscovered by those who study history and know the role of raw milk as a nourishing whole food. Raw milk that is carefully and intentionally produced for direct human consumption is wholly different from milk being produced for pasteurization.
So, the next time that someone says, “milk is for cows and not for humans,” share with them the intricate link between civilization and raw milk, and the competitive advantage that raw milk provided to humanity for 10,000 years. Many of these misinformed humans are in dire need of gut microbiome rescue like never before. Reach out to them with love, compassion and humanity. They need our support, nourishment, and education.