A Farmer’s Takeaways from the 2023 Symposium of the International Milk Genomics Consortium (IMGC)
“If you are the smartest person in the room, you are in the wrong room.”
Introduction
Well…I was in the right room at IMGC with a huge opportunity to learn and grow. Just like all prior years.
The 20th International Milk Genomics Consortium (IMGC) Symposium was held on September 6-8 2023. This was the 12th year that I have attended the IMGC Symposium. For the last several years, the Raw Milk Institute has been an official Bronze Level Sponsor of the conference. These conferences have taken me all over the world, including Cork Ireland, Quebec Canada, Aarhus Demark (twice), Sydney Australia, and UC Davis in California several times. I am nearly always the only farmer in the room filled with dairy processing scientists, PhD students, dairy science professors and university professors, and other milk researchers.
Over 12 years, I have made some great friends and created some important collaborations and alliances. I am approached by PhDs, especially after I speak at the microphone after a particularly engaging presentation that begs questions. They say things like, “Keep on asking those great questions!” I am the only one that can ask those questions because everyone else would potentially lose their NIH or industry grants if they dared to asked those kinds of questions.
Time and interest are ushering in a new generation of open-minded PhD researchers, many of whom are women. They all want to talk about raw milk and its bioactive elements. Raw milk is truly a miracle of nature. Being an event sponsor has allowed greater access to insider information about all things milk. Below are my main takeaways from three intensive days of meetings, interactions, meals and dinner parties, and presentations in Cork Ireland at the University of Cork.
Raw Milk Institute was a Bronze Level Sponsor of the 2023 IMGC Symposium
Raw Milk Nourishes, Protects, and Directs
Raw milk is incredibly complex and perfectly designed to nourish, protect, and direct. We all know that raw milk is designed as the first food of life for babies to thrive and grow, yet as researchers continue to study raw milk, they discover many more benefits.
For instance, raw milk serves as a delivery system for immune-bioactive proteins. Peptides (which are chains of amino acid proteins) are protective of the baby by not allowing pathogens to cause illness. These functional proteins serve many roles, including protection of the baby.
Other specialized-proteins in breastmilk include natural mRNA, which provide the genetic information to direct cellular metabolic processes in the baby. Breastmilk also contains stem cells for repair of damaged cells or tissues.
Raw milk also contains everything needed for its digestion. Raw milk has proteases, peptidases (for digesting proteins), lipases (for digesting fats), and bacteria that make lactase (for digesting lactose).
Additionally, when people drink milk, over time there are changes in the composition of the gut bacteria that make milk digestion easier. Lactase-producing bacteria found in the gut become the probiotic and as they feed on lactose, that becomes their selected prebiotic (food that bacteria chose to digest or eat). Over time the populations of these lactose-loving probiotic bacteria increase when they are fed lactose from dairy products.
The various milk proteins, immunoglobins, enzymes, fats and sugars are “qualitatively similar” between human breastmilk and cow milk. However, they are “quantitatively different” and appear at different levels and amounts in cow milk versus human milk. The same would be true for other bovine milks. The similarities are why humans can drink raw milk from cows, goats, and other animals.
Milk’s Benefits Can’t Be Extracted
Many raw milk researchers are focused on finding ways to extract beneficial elements from raw milk. However, these elements are designed to work together with the full complement of many different macro- and micro- nutrients, enzymes, probiotics, etc in whole raw milk.
New products made with bio-actives extracted from raw milk will likely be met with suspicion, as well they should. The health benefits from whole, raw milk are the result of a complex interplay of bio-actives. Outside of the whole food matrix, those bio-actives are incomplete and not as effective as in their natural state.
Milk Fat is Essential to Its Beneficial Properties
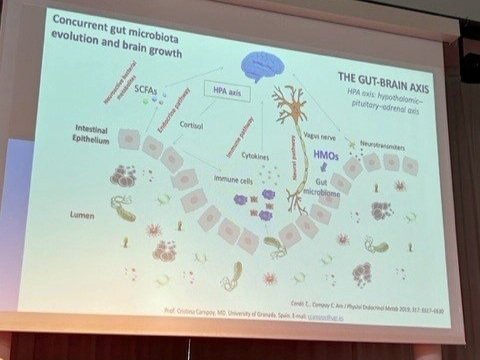
Butterfat in milk is an essential part of milk’s overall beneficial properties. This fat is known to benefit brain development, immune system development, intestinal development, and the composition of the gut microbiota.
Butter fat globules are three-layer thick capsules that come in different sizes. The three-layered capsules are used by the gut as fiber; they also provide butyrate and butyric acids which are highly beneficial and healing to the lower gut. 60% of the bioactive elements found in raw milk are “carried on or inside” the fat globule. This says so much about skim milk, which has lost much of its beneficial value with the removal of the fat.
Researchers discovered that the fat globules in the milk are smaller in cows fed a high energy diet with high stress levels, such as cows being kept in concentrated animal feeding operations (CAFOs). The smaller fat globules in the milk do not contain bacteria inside that could ride through the stomach to the lower gut.
In contrast, the fat globules are larger in cows fed a low energy diet and under low stress levels (such as cows in pasture-based operations). These larger fat globules carry bacteria inside of them. It is thought that the fat cell may act as a protective carrier vessel to carry bacteria though the stomach acid environment into the lower gut where they may be beneficial.
Pasteurization Damages and Denatures Milk
Pasteurization damages milk such that it becomes oxidated, highly allergenic, and hard to digest. It is a common protocol to pasteurize milk up to 3 or 4 times to achieve longer shelf life and assure that the milk is completely dead, with no regard for the essential and beneficial bio-actives that are destroyed in the process.
Raw milk contains everything it needs to digest itself. Raw milk contains enzymes and bacteria that help create more enzymes to digest raw milk and all the sub elements. Milk maldigestion has been over simplified. It is not just lactose; it is the proteins and fats that also need help with digestion.
After pasteurization the bioactive elements needed for milk to digest itself are missing! Fats, proteins, and sugars all need digesting, but their enzymes and digestive bacteria are denatured or dead. Without active enzymes, digestion of fat (via lipase) and proteins (via protease) is inhibited. This results in maldigestion in some consumers.
Whereas raw milk helps to build immune system strength, pasteurized milk does not build up the immune system. Heat denatures the functional proteins and does not allow cellular direction. This can result in cellular confusion and chaos.
Raw whey proteins are highly anti-inflammatory and have many health benefits. The raw whey health benefit findings are consistent with other researchers in the Netherlands, including Dr. Ton Baars’ research on whey proteins showing that they stabilize MAST cells, control histamine release, and reduce allergies.
However, all whey is required to be pasteurized in the USA as per the Food and Drug Administration (FDA) and Pasteurized Milk Ordinance. Whey proteins are destroyed by processing and are highly sensitive to heat. One researcher has been frustrated in trying to extract the beneficial components from pasteurized whey. The heating of whey makes the components “sticky” such that they plug up the ultrafiltration micropores. Therefore, ultra filtration cannot be used to extract whey components from pasteurized whey.
New Pasteurization Technologies Cause Less Damage Than Traditional Heat Pasteurization
As an alternative to heat-based pasteurization, researchers are studying other methods such as high pressure (HPP), ultrafiltration, and ultraviolet (UV) light. These methods are effective at inactivating bacteria and less harmful to milk than heat-based pasteurization. For instance, both high pressure processing and ultraviolet processing preserve some of the bioactive milk proteins better than heat-based pasteurization.
Nonetheless, milk processors in the USA are resisting the use of these new technologies. In some other countries, UV and HPP are being successfully used, but in the USA the FDA continues to represent processors’ interests and thereby block the ability to innovate with these alternatives to heat processing. This failure to innovate with HPP, UV or Ultrafiltration is creating a loss of consumer interest in pasteurized milk as people continue to suffer from maldigestion when consuming pasteurized milk.
In Studies, 20,000+ Kids Drank Raw Milk With NO Milk-Related Illnesses
The pioneering PARSIFAL and GABRIELA studies of more than 55,000 kids in Europe really set the international high bar for studies on raw milk. The overall findings included reduced rates of asthma, eczema, respiratory illnesses, fevers, allergies, and ear infections in children who drank raw milk.
At the symposium, it was emphasized that during all of those studies and over twenty years of research, there was never a “red flag event.” A red flag event would be a reported illness from raw milk consumption. The studies included data from more than 20,000 children who drank raw milk, and there was not a single red flag event!
Yet, at the end of each of the peer reviewed and journal published articles, there is a disclaimer that says something such as, “even though there are health benefits to consuming raw milk, the researchers can not recommend raw milk because of the risks of raw milk consumption.” This disclaimer was included because peer review and journal publication political pressures demanded it, despite the fact that there was no basis in the research data.
Dr. Markus Ege MD and Mark McAfee, in Cork Ireland at the IMGC symposium 2023
Raw Milk Provides Sustainability for Farmers and Superb Nutrition for Consumers
Farmers have been denied fair markets for their dairy products for more than a century. All of the value-added efforts are happening after products leave the farm. Milk processors continue to ensure that farmers are paid low prices for their milk, resulting in the loss of thousands of family farms. However, raw milk provides a pathway to sustainability and life satisfaction for dairy farmers.
Raw milk presents a unique farmstead product that brings all the added value back to the farmer with an incentive to work on quality. By selling directly to consumers, raw milk farmers are able to obtain greater financial rewards for their work, while consumers benefit from the improved flavor and nutrition. It’s a win-win for farmers and consumers!
Raw milk that is carefully and intentionally produced for direct human consumption is a low-risk food. This type of raw milk is wholly different from raw milk being produced in unhygienic conditions. Raw milk intended for direct human consumption is produced in sanitary conditions, with much care to ensure that the animals are healthy and that the milk is clean. This type of raw milk is tested often and held to rigorous standards to ensure that it is being produced in a way that discourages pathogen growth.
By combining nature’s blueprints, the bio-actives found in whole raw milk, standards for good production practices and modern testing systems, RAWMI Listed farmers are nourishing consumers safely. Congrats to all of the RAWMI Listed pioneers!