References
[1] Liu, J., Zhu, Y., Jay-Russell, M. et al. (2020) Reservoirs of antimicrobial resistance genes in retail raw milk. Microbiome 8, 99 (2020). https://doi.org/10.1186/s40168-020-00861-6
[2] Durso LM, Miller DN, Wienhold BJ (2012) Distribution and Quantification of Antibiotic Resistant Genes and Bacteria across Agricultural and Non-Agricultural Metagenomes. PLOS ONE 7(11): e48325. https://doi.org/10.1371/journal.pone.0048325
[3] Wright, G. (2007) The antibiotic resistome: the nexus of chemical and genetic diversity. Nat Rev Microbiol 5, 175–186 (2007). https://doi.org/10.1038/nrmicro1614
[4] Ben Maamar S, Glawe AJ, Brown TK, Hellgeth N, Hu J, et al. (2020) Mobilizable antibiotic resistance genes are present in dust microbial communities. PLOS Pathogens 16(1): e1008211. https://doi.org/10.1371/journal.ppat.1008211
[5] Fogler K, Guron GKP, Wind LL, Keenum IM, Hession WC, Krometis L-A, Strawn LK, Pruden A and Ponder MA (2019) Microbiota and Antibiotic Resistome of Lettuce Leaves and Radishes Grown in Soils Receiving Manure-Based Amendments Derived From Antibiotic-Treated Cows. Front. Sustain. Food Syst. 3:22. doi: 10.3389/fsufs.2019.00022
[6] Pärnänen, K., Karkman, A., Hultman, J. et al. (2018) Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat Commun 9, 3891. https://doi.org/10.1038/s41467-018-06393-w
[ 7] Ravindran S. (2019) Breastfeeding May Help Protect Babies from Antibiotic-Resistant Bacteria. SPLASH! milk science update: January 2019 Issue. https://milkgenomics.org/article/breastfeeding-may-help-protect-babies-from-antibiotic-resistant-bacteria/
[8] Rova S, Rada V, Marsik P, Vlkova E, Bunesova V, Sklenar J, Splichal I. (2011) Growth of bifidobacteria and clostridia on human and cow milk saccharides. Anaerobe 17(5). https://doi.org/10.1016/j.anaerobe.2011.07.009.
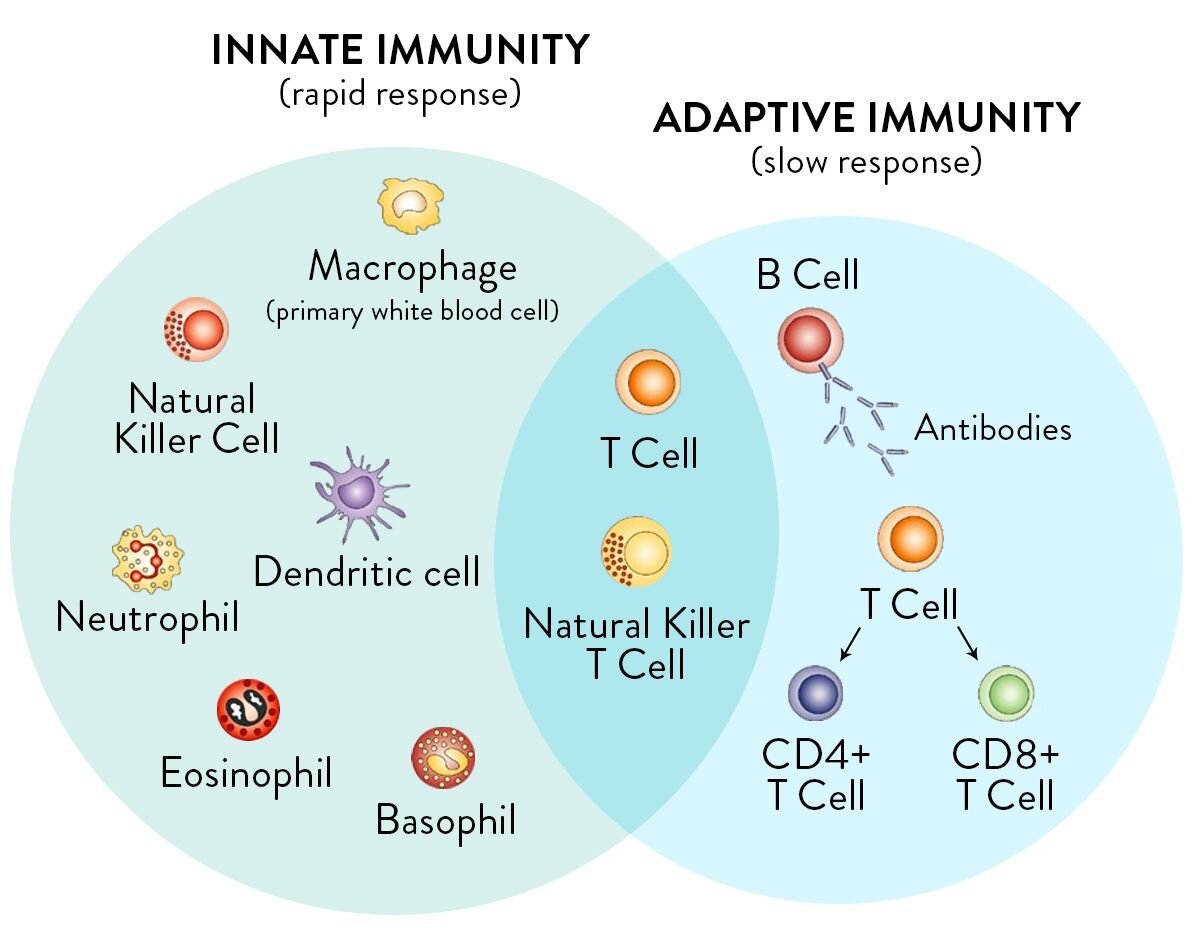
[9] McAfee M, Smith S. (2020) Immunity, the Immune System, and Raw Milk. Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/immunity-the-immune-system-and-raw-milk
[10] Centers for Disease Control and Prevention. (2019) More People in the United States Dying from Antibiotic-Resistant Infections than Previously Estimated. CDC website. https://www.cdc.gov/media/releases/2019/p1113-antibiotic-resistant.html
[11] Brandt L. J. (2012). Fecal transplantation for the treatment of Clostridium difficile infection. Gastroenterology & hepatology, 8(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3365524/
[12] Akst, J. (2020) The influence of soil no immune health. The Scientist website. https://www.the-scientist.com/news-opinion/the-influence-of-soil-on-human-health-66885
[13] Wells, AD, Poole JA, and Romberger DJ. (2014) Influence of farming exposure on the development of asthma and asthma-like symptoms. International immunopharmacology, 23(1), 356–363. https://doi.org/10.1016/j.intimp.2014.07.014
[14] Levi, J. (2014) The Smoke Cured Fermented Milk of the Samburu. Presentation at Wise Traditions London 2014. https://westonaprice.london/videos/samburu/
[15] Smith, S. (2020) Udder Preparation for Raw Milk. Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/udder-preparation-for-raw-milk
[16] Bourrie BC, Willing BP, and Cotter PD. (2016) The Microbiota and Health Promoting Characteristics of the Fermented Beverage Kefir. Frontiers in microbiology, 7, 647. https://doi.org/10.3389/fmicb.2016.00647
[17] Bellikci-Koyu E, Sarer-Yurekli BP, Akyon Y, Aydin-Kose F, Karagozlu C, Ozgen AG, Brinkmann A, Nitsche A, Ergunay K, Yilmaz E, and Buyuktuncer Z. (2019) Effects of Regular Kefir Consumption on Gut Microbiota in Patients with Metabolic Syndrome: A Parallel-Group, Randomized, Controlled Study. Nutrients, 11(9), 2089. https://doi.org/10.3390/nu11092089
[18] Guzel-Seydim ZB, Kok-Tas T, Greene AK, Seydim AC. (2011) Review: functional properties of kefir. Crit Rev Food Sci Nutr. 51(3):261-268. doi:10.1080/10408390903579029
[19] de Oliveira Leite AM, Miguel MA, Peixoto RS, Rosado AS, Silva JT, and Paschoalin VM. (2013) Microbiological, technological and therapeutic properties of kefir: a natural probiotic beverage. Brazilian journal of microbiology : [publication of the Brazilian Society for Microbiology], 44(2), 341–349. https://doi.org/10.1590/S1517-83822013000200001
[20] Berge AC, Baars T. (2020) Raw milk producers with high levels of hygiene and safety. Epidemiology and Infection. 148:e14. doi:10.1017/S0950268820000060
[21] Loss G, Apprich S, Waser M, Kneifel W, Genuneit J, Büchele G, Weber J, Sozanska B, Danielewicz H, Horak E, Joost van Neerven RJ, Heederik D, Lorenzen PC, von Mutius E, Braun-Fahrländer C; GABRIELA study group. (2011) The protective effect of farm milk consumption on childhood asthma and atopy: The GABRIELA study. Journal of Allergy and Clinical Immunology. 128 (4): 766-73. https://www.jacionline.org/article/S0091-6749(11)01234-6/fulltext
[22] Perkin MR and Strachan DP. (2006) Which aspects of the farming lifestyle explain the inverse association with childhood allergy? Journal of Allergy and Clinical Immunology. 2006; 117 (6):1374-81. https://www.jacionline.org/article/S0091-6749(06)00651-8/fulltext
[23] Loss G, Depner M, Ulfman LH, Joost van Neerven RJ, Hose AJ, Genuneit J, Karvonen M, Hyvärinen A, Kaulek V, Roduit C, Weber J, Lauener R, Pfefferle PI, Pekkanen J, Vaarala O, Dalphin JC, Riedler J, Braun-Fahrländer C, von Mutius E, Ege MJ; PASTURE study group. (2015) Consumption of unprocessed cow's milk protects infants from common respiratory infections. Journal of Allergy and Clinical Immunology. 135 (1): 56-62. https://www.jacionline.org/article/S0091-6749%2814%2901274-3/fulltext
[24] Watanabe K, Gilchrist CA, Uddin J, Burgess SL, Abhyankar MM, Moonah SN, Noor Z, Donowitz JR, Schneider BN, Arju T, Ahmed E, Kabir M, Alam M, Haque R, Pramoonjago P, Mehrad B, Petri WA. (2017) Microbiome-mediated neutrophil recruitment via CXCR2 and protection from amebic colitis. PLOS Pathogens; 13 (8): e1006513 DOI: 10.1371/journal.ppat.1006513
[25] Paula Neto HA, Ausina P, Gomez LS, Leandro JGB, Zancan P, Sola-Penna M. (2017) Effects of Food Additives on Immune Cells As Contributors to Body Weight Gain and Immune-Mediated Metabolic Dysregulation. Front Immunol.8:1478. doi:10.3389/fimmu.2017.01478
[26] McAfee M. (2020) Build Immune System Strength With Whole Foods: Drink Raw Milk! Raw Milk Institute website. https://www.rawmilkinstitute.org/updates/whole-foods-build-immune-system-strength