My family has been drinking raw milk for over 18 years. I drank raw milk through both of my pregnancies and raised both of my kids on raw milk since they were weaned from breastmilk as toddlers. I have purposely chosen raw milk for my family because of its exceptional health benefits and animal welfare.
Studies performed in Europe have shown that children who drink raw milk have decreased rates of asthma, allergies, eczema, ear infections, fever, and respiratory infections. Nonetheless, when I tell people that my family drinks raw milk, I often hear responses such as:
“Raw milk is dangerous!”
“Doesn’t raw milk make people sick?”
“I heard that raw milk was bad for you.”
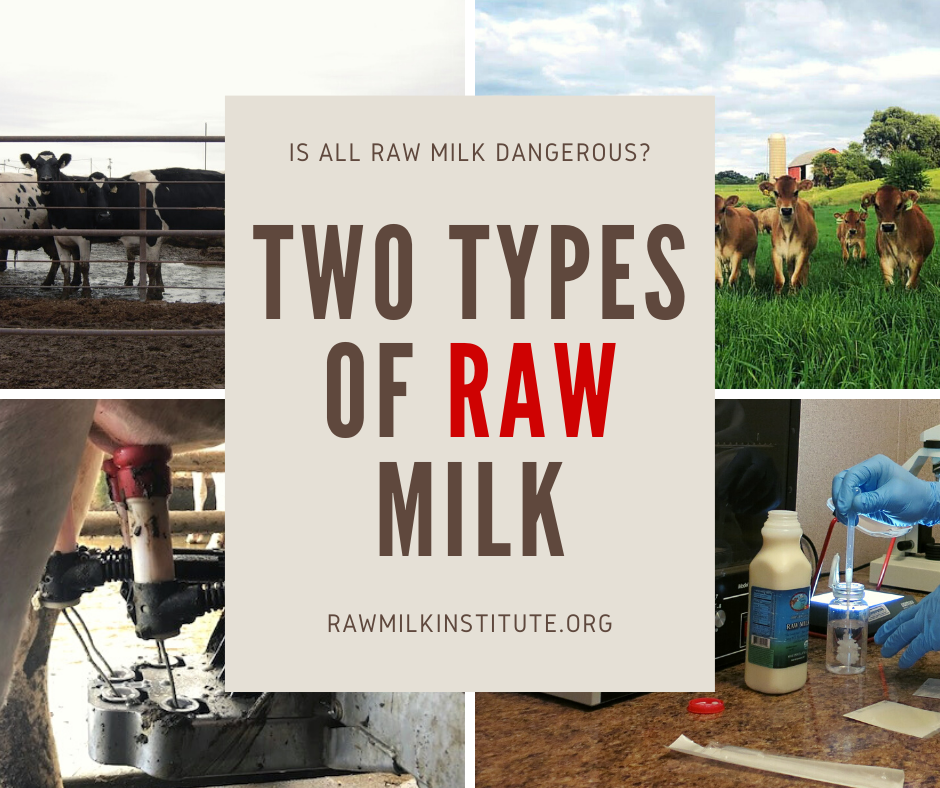
The reason for raw milk’s negative reputation is that there are two types of raw milk! Raw milk that is intended for pasteurization is quite different than raw milk produced for direct human consumption.
Raw Milk Intended for Pasteurization
When my family drives past a nearby dairy that produces milk for pasteurization, we are struck by the horrendous smell and filthy living conditions. The animal yard is completely covered with manure. The cows have no choice but to lie and stand in manure all day. It is disgusting to think that this operation is producing food for families.
Raw milk that is “intended for pasteurization” is typically sourced from Concentrated Animal Feeding Operations (CAFOs). This type of milk is actually defined under the Federal Grade A Pasteurized Milk Ordinance (PMO). Such milk is being produced in conditions where animal health is often compromised and mastitis (udder infection) is common. Antibiotics are often utilized in these herds, and hormones are used to stimulate higher levels of milk production. The animals are housed in an abundance of manure, and there is a corresponding high rate of pathogens.
This milk is intended to be pasteurized to kill pathogenic bacteria, and as such, it is often produced with little care towards preventing contamination with pathogens. Furthermore, this type of milk is generally commingled with milk from multiple dairies, which increases the risk of pathogenic exposure. Studies have shown that up to 33% of this type of milk tests positive for pathogens. This type of raw milk is clearly unsafe to consume. I would never feed this type of raw milk to my family.
Raw Milk Intended for Direct Human Consumption
When my family visits the dairy that produces the raw milk that we drink, we see a very different setting from the CAFO dairy. The cows at the raw milk dairy are happily grazing on lush pastures. The cows look clean and healthy. The milk is bottled on-farm, and we can see that the milk bottling room is clean and neat. There is a stark contrast between the CAFO dairy and this raw milk dairy.
Raw milk that is carefully and intentionally produced for direct human consumption is wholly different from raw milk being produced for pasteurization. Raw milk farmers carefully manage the cleanliness and hygiene of the farm from grass-to-glass, with much care to ensure that the animals are healthy and the milk is clean.
From the health of the herd, to cleanliness of the milking parlor, to the specific cleaning processes for the milk line, to ensuring rapid milk chilling, to regularly testing their milk, and everything in between, raw milk farmers are dedicated to taking their farm management to the next level in order to ensure that their raw milk is safe to consume.
Although there are no federal standards for raw milk, the Raw Milk Institute has established Common Standards for raw milk that is intended for direct human consumption. This type of raw milk is tested often and held to rigorous standards to ensure that it is being produced in a way that discourages pathogen growth.
Where Do Pathogens in Milk Originate?
The four main pathogens in milk that can cause human illness are E coli 0157:H7, listeria mono, salmonella, and campylobacter. The two most common sources of pathogens in milk are manure and mastitis. It is estimated that one-third of CAFO dairy cows have mastitis, and the cows in CAFOs stand and lie in manure all day. Clearly, this type of dairy environment is primed for pathogen growth.
On the other hand, the raw milk dairy environment is carefully managed to prevent pathogens in the milk. These farmers manage the health of their herd to prevent mastitis. They ensure that the milk from any animals that are showing signs of mastitis is not used for direct human consumption. Raw milk farmers meticulously clean the udders before milking to ensure that no manure or other contaminants are present. They also rigorously and frequently clean their milking machines, milk lines, and milk tanks.
Take a look at the milk filters shown below. Even with just a quick look, it is apparent that the milk being produced with the intent to be pasteurized is clearly not clean, whereas the milk filter from the intentionally-produced raw milk looks impeccable. (To be fair, there are some dairy farmers who produce milk for pasteurization that is much more hygienic than most others. However, that milk is still commingled with milk from other dairies, many of which are likely to not use hygienic practices.)
Comparison of Bacterial Test Standards for Two Types of Raw Milk
Okay, I’m gonna get technical here. If reading about standards and looking at charts is not your thing, you can skip ahead to the last section. :)
Two important types of bacterial testing for milk are Standard Plate Count (SPC) and coliform count. The SPC is a measure of the total number of aerobic bacteria in the milk. High SPC numbers can indicate dirty milking equipment, poor milk chilling, and/or poor udder preparation.
Coliform count measures the amount of coliform bacteria present in the milk. Coliform counts measure the overall hygiene and cleanliness of the milk. High coliform counts generally indicate the presence of manure or other environmental contaminants on the udders or milking equipment. High coliform counts are likely to correspond to the presence of pathogens in the milk.
According to the PMO, pre-pasteurized milk is allowed to have up to 100,000 colony-forming units (cfu) of bacteria per mL in SPC testing. The PMO does not have a standard for how many coliforms are allowed in pre-pasteurized milk, but the state of California allows coliforms up to 750 cfu/mL of milk.
In comparison, the Raw Milk Institute Common Standards call for <5,000 cfu/mL for SPC testing, and <10 cfu/mL in coliform testing. As you can see in the chart below, intentionally-produced raw milk is measurably quite different from pre-pasteurized raw milk, and even meets stricter standards than pasteurized milk.
The Raw Milk Institute has been collecting monthly Standard Plate Count and Coliform Count data from its LISTED raw milk dairies since 2012. This dataset of thousands of test results shows that raw milk farmers who have been properly trained can routinely meet the stringent standards set forth in the Common Standards.
Research on Raw Milk Safety
Researchers from Canada and Europe have studied the safety of raw milk intended for direct human consumption. They have found that carefully produced raw milk is a low-risk food which is fundamentally different from pre-pasteurized milk.
The table below contrasts pathogen test data from pre-pasteurized milk vs. raw milk intended for direct human consumption. As illustrated in the table, pathogen testing of pre-pasteurized milk samples has detected pathogens in up to 33% of samples. In contrast, there were zero pathogens detected in thousands of milk samples from raw milk intended for direct human consumption. It is clear from this test data that pre-pasteurized milk is categorically different from raw milk intended for direct human consumption.
Data courtesy of the British Columbia Herdshare Association
Not All Raw Milk Is Dangerous!
It is clear that raw milk produced with the intention to be pasteurized is likely to contain dangerous pathogens. This type of raw milk is unsafe, and I would never feed it to my family. Unfortunately, this type of raw milk’s negative reputation has led many to believe that all raw milk is unsafe to consume.
It is important to note that there is no such thing as a perfectly safe food. An analysis of foodborne illnesses from 2009-2015 showed that the top food categories commonly linked to illnesses were chicken, pork, and seeded vegetables. Pasteurized milk is not perfectly safe, either, and is implicated in foodborne illnesses and outbreaks every year. The CDC outbreak and illness data which is used to assert that raw milk is unsafe does not distinguish raw milk intended for pasteurization from raw milk that is carefully produced and intended for direct human consumption.
It is clear from the above-presented test data that intentionally-produced raw milk is a low-risk food. In my family, we purposely choose raw milk for its superior nutrition and significant health benefits over pasteurized milk. Raw milk contains greater bioavailable nutrients than pasteurized milk, as well as a wide array of beneficial enzymes and probiotics which are known to have benefits on the immune system and gastrointestinal tract.